💡Important for You
WEGOVITA offers medical coordination services by connecting international patients with top hospitals and specialists across Germany. We support access to expert evaluations, facilitate treatment logistics, and present a range of available medical options.
However, WEGOVITA does not provide direct medical treatment, make medical diagnoses, or recommend specific therapies. All final medical decisions—including diagnosis, treatment planning, and cost—are made solely by licensed medical professionals after a full clinical assessment of the individual patient.
This information is provided for informational purposes, based on internationally recognized guidelines and practices used in Germany’s leading medical institutions. It is not a substitute for professional medical advice.
💡 Interested in clinical trial references, treatment innovations, or cost comparisons? Contact our medical coordination team at info@wegovita.com for personalized assistance.
Your Health. Your Journey. With WEGOVITA.



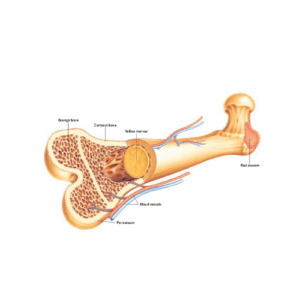
 Red blood cells (RBCs): Transport oxygen from the lungs to tissues and remove carbon dioxide. A lack of RBCs leads to anemia, causing fatigue, dizziness, and shortness of breath.
Red blood cells (RBCs): Transport oxygen from the lungs to tissues and remove carbon dioxide. A lack of RBCs leads to anemia, causing fatigue, dizziness, and shortness of breath. Blood Cancers (Leukemia & Lymphoma): The uncontrolled growth of cancerous blood cells replaces normal bone marrow function, preventing the production of healthy cells.
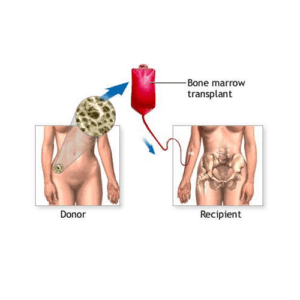
Blood Cancers (Leukemia & Lymphoma): The uncontrolled growth of cancerous blood cells replaces normal bone marrow function, preventing the production of healthy cells. Looking for a bone marrow transplant in Germany?
Looking for a bone marrow transplant in Germany? University Hospital Heidelberg – A leader in stem cell transplantation and leukemia research.
University Hospital Heidelberg – A leader in stem cell transplantation and leukemia research. Autologous BMT: ~50–70% 5-year survival rate (used in specific cases for consolidation therapy).
Autologous BMT: ~50–70% 5-year survival rate (used in specific cases for consolidation therapy).


 Patient: Julia, 28 (Acute Myeloid Leukemia – AML)
Patient: Julia, 28 (Acute Myeloid Leukemia – AML) Patient: Amir, 9 (Sickle Cell Disease)
Patient: Amir, 9 (Sickle Cell Disease) Patient: Mark, 54 (Multiple Myeloma – Stage III)
Patient: Mark, 54 (Multiple Myeloma – Stage III)
 Email:
Email:  Website:
Website:  Phone/WhatsApp:
Phone/WhatsApp:  Health is Your Journey with WEGOVITA
Health is Your Journey with WEGOVITA Sources & References Used in This Article
Sources & References Used in This Article European Society for Blood and Marrow Transplantation (EBMT) – Clinical guidelines for patient eligibility and treatment.
European Society for Blood and Marrow Transplantation (EBMT) – Clinical guidelines for patient eligibility and treatment.